Sponsored Content
In this interview, DTC Perspectives’ Chairman, Bob Ehrlich, and Phreesia’s SVP of Life Sciences, David Linetsky, discuss how the patient experience has evolved rapidly during the COVID-19 pandemic, particularly as providers leverage digital patient intake solutions to enable safer contactless workflows. They will also explore the importance of aligning with platforms that are flexible, adaptive, and meet patients where they are, given that these changes are likely here to stay.

Bob Ehrlich: As many are aware, the outbreak of the COVID-19 pandemic resulted in steep declines in office visit volumes in the Spring. Phreesia has since published multiple studies on outpatient visit volumes with Harvard University and the Commonwealth Fund, using Phreesia’s network data. Can you provide some insight into where these visit trends now stand?
David Linetsky: Bob, I am happy to report that overall, patients have returned to seeking care. Most practices within the Phreesia network appear to have adapted to the pandemic and stabilized their operations. Visit volumes have remained relatively stable since June and in many cases have returned to pre-pandemic levels. In some cases, visit volumes have even exceeded their pre-pandemic levels, as many practices do active outreach to their patient populations to bring them in to catch up on deferred care.
Phreesia continues to publish this data in partnership with researchers from Harvard and the Commonwealth Fund. Our reports are released monthly and can be found on the Commonwealth Fund’s website.
Bob: I am glad to hear that levels are approaching normal. Phreesia has released several applications as a response to the pandemic across its provider network. As medical offices adjust to the “new normal”, how have these digital intake solutions helped practices get their visit volumes back to pre-pandemic levels?
David: Practices are implementing contactless workflows that help minimize exposure between patients and staff. Phreesia’s Zero-Contact Intake offering allows practices to set up alternative workflows, such as patients checking in from their cars or drive-through testing sites. In addition, practices are removing unnecessary shared spaces and assigning many of their non-provider staff members to remote work. Our COVID-19 Screening Module also automatically screens patients for self-reported COVID-19 risk factors before their visits and is continually updated based on evolving CDC guidance.
Telehealth visits have been proven to be an essential solution for patients, allowing those who don’t need to be seen in person to continue to receive care. Phreesia’s Intake for Telehealth workflow captures important intake information ahead of the visit and facilitates the start of the virtual session.
We recognized the urgent need for intake products that could support telehealth visits, screen for COVID-19 risks and minimize contact during in-person visits, and we shifted our efforts to help medical groups stay safe, stay open and continue to see patients.
Bob: Telemedicine seems to have been breaking new ground in providing a safe and efficient alternative for patients. How do you view this solution long-term?
David: We’ve heard from many of our practices that their priority is to adapt to COVID-19 by putting the safety of providers, medical staff and patients first. Prior to COVID-19, the telehealth market was dominated by specialty services offered through employee benefits plans. With the expansion of visit types qualifying for telehealth reimbursement and Medicare copays waived for telehealth visits, many of the barriers that have traditionally prevented practices from embracing virtual visits have been removed.
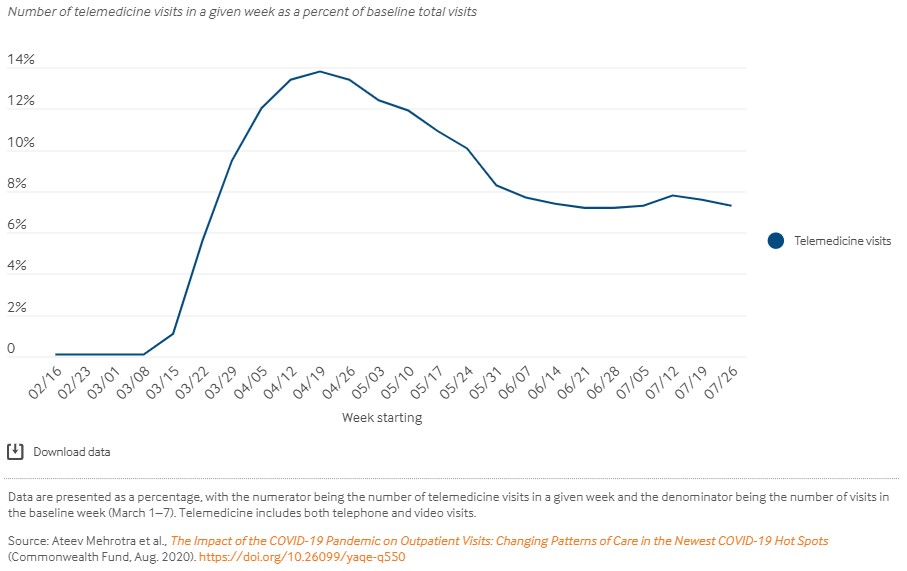
Data from our most recent Commonwealth Fund report show that while telehealth adoption varies significantly depending on the specialty, telehealth utilization has been relatively stable since June, at a level many times higher than pre-pandemic.
While the future of reimbursement changes—and therefore of telehealth—remains uncertain, many providers are looking towards telehealth as a creative, long-term solution to deliver patient care. From portable EKG machines to at-home ultrasounds to cancer screenings, physicians are looking for effective alternatives to traditional in-person services.
Bob: Do you see COVID-19 as the initial cause of these changes to the patient experience, or do you think some of these changes were already underway prior to the pandemic?
David: That’s a great question. While the COVID-19 outbreak accelerated the adoption of these tools among providers, it was not the initial catalyst. Prior to the pandemic, many healthcare providers had already begun to adopt digital engagement tools to manage operational, clinical and financial processes. This is a change that has been happening for many years in other industries, with consumers having come to expect the convenience of digital solutions broadly. So, safety concerns have greatly accelerated these changes in healthcare, but those changes were already underway and they will persist because consumers expect effective and convenient options.
Phreesia’s patient intake platform was designed to support these trends, which has allowed us to thrive in the current industry environment and to deliver valuable applications to our provider network and the broader market. As we navigate a new normal in a post-COVID-19 world, we believe digital engagement tools will become even more critical to ensuring that the POC stays relevant to Life Sciences manufacturers and healthcare marketers.
Bob: With all these changes in the patient experience rapidly occurring, do you think Point of Care is still an effective channel to engage with patients?
David: Absolutely. Point of care remains a critical and incredibly valuable channel. However, to be successful, healthcare marketers must adapt to the long-term changes to the patient experience. They must understand that the point of care continues to become more ephemeral and less tied to physical locations; it’s now wherever patients choose to engage with their providers and seek care. In addition, one-to-one engagement tactics are increasingly more valuable as in-person visit volumes fluctuate because of COVID-19. Marketers should not have to worry about audience volume or quality. They should focus on tactics that ensure both of those important factors.
Some traditional tactics are quickly becoming obsolete due to providers’ concerns about shared surfaces. As technology enables patients to take an even more active role in their care, patients are increasingly receptive to personalized content tailored to their individual health needs, that can be accessed on their own devices.
Lastly, COVID-19 has caused a tremendous disruption to patients’ access to care, creating a greater need for support programs. The point of care has moved beyond the walls of the physician’s office, and I believe that the POC marketing industry must adapt.
Bob: Are there specific strategies you suggest for the Point of Care marketing industry to adapt to the increasingly digital environment?
David: I believe it is critical for healthcare marketers and life sciences manufacturers to have strategic insight into how the POC can become an integral part of their digital and mobile strategy. Patient utilization data demonstrate the value of mobile and how it enables providers to deliver care safely through contactless and virtual workflows. Personalized content and directed, one-to-one engagements cut through the noise and influx of health information and address patients’ specific needs and priorities.
Finally, incorporating disease education and patient support programs into digital engagement campaigns to ultimately improve health outcomes for target patient populations will be critical for long-term success in the changing healthcare landscape. As the patient experience becomes increasingly mediated by the converging forces of digital adaptation, patient centricity and pandemic response, we must find a way to align our digital engagement strategies at the point of care to every patient’s needs.
About David Linetsky
SVP, Life Sciences, Phreesia
David Linetsky is responsible for cultivating Phreesia’s partnerships with Life Sciences companies, supporting them in the development of healthcare products that deliver value and engage patients in their care. He has worked at Phreesia for more than a decade and held key leadership roles, including Vice President of Analytics and Insights, and Vice President of Finance.
Prior to joining Phreesia, David worked in academia as a researcher and instructor in the fields of biotechnology, mathematics and philosophy. David holds a BS in mathematics from the University of Alberta. He also earned a master’s degree and was a PhD candidate in mathematics and logic at the City University of New York.
To learn more about Phreesia, please click here or visit them on: